Hospital Readmissions
Hospital readmissions have recently come into the spotlight in the US as many hospitals came under pressure to limit their readmission numbers. Groups like the Centers for Medicaid and Medicare Services (CMS) have started imposing penalties on hospitals that have high levels of readmission in their Medicare/Medicaid patient populations, and other insurers are likely to follow their example. This is encouraging many healthcare providers to find new and innovative ways to help reduce readmissions.
So what is a “hospital readmission”?
A hospital readmission occurs when a patient who is treated in a hospital and is discharged returns to the hospital within 30 days of that first visit for the same condition as their original hospital visit. CMS focuses on high risk conditions that put patients at risk for recurring complications, including pneumonia, heart failure, heart attack, chronic lung problems such as emphysema and bronchitis (COPD), and elective hip and knee replacements.
Why is this important?
Readmissions generally occur as a result of preventable errors and communication failures following discharge. These can cause complications related to the illness, and patients end up back in hospital, with more damage to their health.
Why do we have high levels of hospital readmissions?
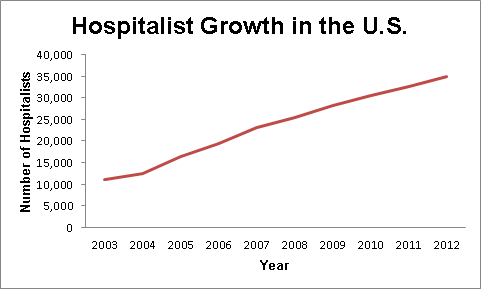
Prior to the 1990’s when a patient was admitted to hospital their family physician (primary care physician, or “PCP”) would come to the hospital morning and evening, taking normal clinic hours during the day. They would “round” on their patients with the hospital care team, writing new prescriptions and making treatment decisions. In 1996, the term “hospitalist” was coined, referring to a new type of medical practitioner who is in charge of patient care inside the hospital, but is not involved in the day-to-day treatment of patients when they return home. Over the last 20 years, the number of PCPs that still attend the hospital to provide care to their hospitalized patients has dwindled, with few maintaining hospital privileges, instead allowing for rapid growth of hospitalists to manage care. In 1997, there were only 23 registered hospitalists. Today, there are over 40,000 currently practicing in the U.S.
Because of this skyrocketing trend, many PCPs may not even know their patients have been hospitalized.
Hospitalists often have training in internal medicine, and may have advanced training in managing critical illnesses. Because they work inside the hospital, they are often available 24 hours a day, making it easier for them to respond to any changes the patient experiences. This also means that patients will often be under the care of 2 or more hospitalists during their hospital stay. Hospitalists develop special skills for managing serious illnesses because they are in the hospital all the time, but their understanding of community resources and care at home may be limited. This means that the transition to home care is an incredibly important time for the patient, as all the changes the hospitalist made to their care must be communicated to their PCP and their pharmacy.
Hospitalist care has grown quickly because hospitals are under more pressure to save money and discharge patients earlier, while maintaining safety and quality of care. There is good evidence to show that hospitalists are able to provide the same quality of care, while decreasing the length of a hospital stay for patients, putting them at lower risk for hospital acquired problems.
While patients still receive good care in the hospital, all these changes mean that when they leave the hospital there is a lot more room for error, as their PCP will not know what changes there have been and what happened. This means that there is a greater risk of patients being readmitted to hospital, often for the same reason as their same hospitalization.
Because of these issues with what is termed “continuity of care” there is a drive to improve the management of these transitions.Hospitals now have teams of healthcare workers dedicated to educating their patient about their transition home, however these teams focus on providing information to the patient, and often fail to talk to the PCP or pharmacy. There can often be a lot of new information that is harder to follow, especially for someone who is only just recovering, so it is important all community healthcare providers know how best they can support their patient.
How are our local hospitals doing ?
According to the Centers for Medicare & Medicaid Services, the national average for all cause readmission rates is 15.2% for readmission related to internal medicine, surgery/gynecology, cardiorespiratory, cardiovascular and neurology services. Most local hospitals performed at the national average, that is they did not show a statistically different level of readmissions. Two hospitals in our local area stand out:
- UNC 16.6% – Worse than national average
- WakeMed Raleigh 13.5% – Better than national average
For higher risk conditions the readmission rates are higher. With COPD, a high risk condition, the national average shows that 20.2% of patients are readmitted to hospital within 30 days of an initial hospitalization. Local hospitals all perform approximately the same as the national average, but this still means that one in five people admitted to hospital with a COPD flare will return within 30 days.
Patients may also be discharged to a rehabilitation (rehab) or short-term nursing facility. This creates another step that could create confusion with patient’s medications and treatments.
What are local healthcare providers doing to help prevent readmissions?
Health Park Pharmacy created a new standard of care for patients in transition with a pilot program that we call Project Harmony. We are currently working with Southern Long Term Care Facilities (Sunnybrook,Raleigh Rehab, Zebulon & Petigrew), Duke Raleigh Hospital, Aware Senior Care & WellCare to keep our patients safe as they move from one level of care to another
Project Harmony
Project Harmony aims to overcome the inadequate communication between primary care physicians, hospitals, specialists and pharmacists. It uses a simple and logical approach to address the communication deficits using a simple stepwise approach to the problem.
- The facility sends us a list of your medications
- These medications are placed in easy to use compliance packaging and delivered to your home the day of discharge
 We share that medication regimen with your primary care physician
We share that medication regimen with your primary care physician
While national readmission rates currently remain around 20% for high risk conditions, Project Harmony has been able to show a drastic improvement in readmission with a rate of 6.25%. Patients enrolled in Project Harmony have an average of 15 prescriptions per patient.
Anyone can recommend a patient for Project Harmony. If you know someone leaving the hospital and you are worried about the transition home, reach out to Health Park Pharmacy at (919) 847-7645.
Other programs operating locally to help with transition include Well Care Solutions. Well Care Solutions are providers of specialized quality home healthcare, with a range of services, including:
- Home Care Assistance – short and long term in-home care
- Errands, household duties, personal care services, meal preparation, companionship, exercising assistance, sitter services, incontinence care, private duty nursing
- Nursing – medical assistance and healing at home
- skilled nursing, physical therapy, occupational therapy, speech therapy, medical social worker, wound care, orthopedic program, heart disease management, dementia & alzheimer’s care
- Additional Services
- Telehealth – an easy to use monitoring system that, when placed in the home, will provide daily vital signs, monitoring and intervention opportunities, which will increase overall continuity of care.
- LifeAid – an Emergency Response System. You simply press the button on your waterproof wristband or necklace and you will get a live person on the phone.
- Alert Response Medication System – visual and audio alerts including via phone call to remind you to take your medication on time.
Visit wellcarehealth.com if this sounds like something that may benefit you or a loved one.
Written by: Erin Brown, PharmD Candidate, UNC
Jonathan Wall, PharmD Candidate, Campbell University